Role of Ursodeoxycholic Acid in the Treatment of Liver Cirrhosis
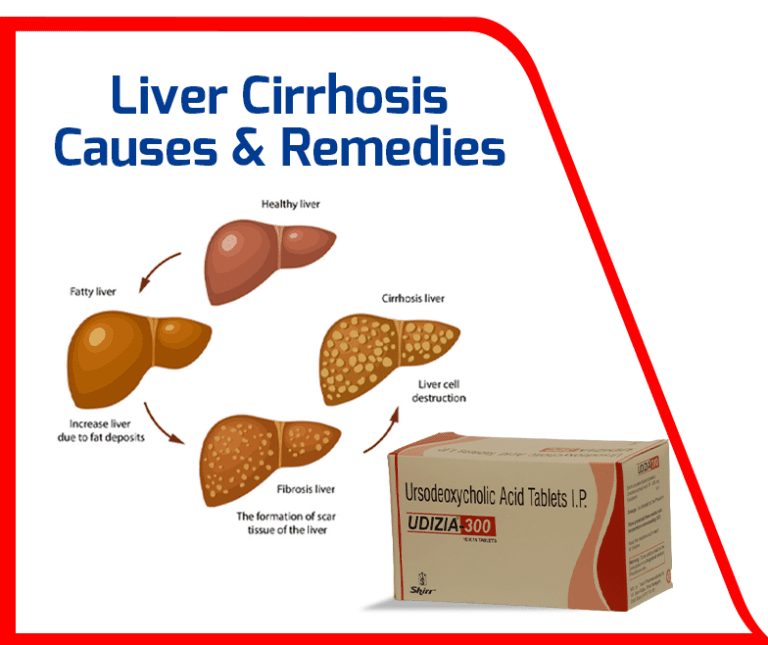
Liver cirrhosis is a form of disorder of your liver, with severe scarring or fibrosis brought on by several diseases and ailments of the liver, including hepatitis and chronic alcoholism.
Liver cirrhosis is a form of disorder of your liver, with severe scarring or fibrosis brought on by several diseases and ailments of the liver, including hepatitis and chronic alcoholism. Your liver strives to heal itself whenever it sustains damage from a disease, excessive alcohol use (binge drinking), or other causes. The result of liver disease and its complications is normally cirrhosis. The scar tissue minimizes the liver’s ability to handle nutrients, hormones, medicines, and natural toxins and limits blood flow through the liver. Additionally, it reduces the liver’s ability to synthesize proteins and other materials.
For more information on UDIZIA 300 . Click on the image above —>
With time, cirrhosis affects the normal functioning of the liver. Cirrhosis is fatal in later stages. Hepatitis B and C infections, excessive alcohol consumption, and fatty liver brought on by diabetes and obesity are among the common causes. During the early stages of cirrhosis, you might not experience any symptoms. In India, around 10 lakh new liver cirrhosis cases are reported yearly; it’s 274 new cirrhotic cases daily. The World Health Organization ranks it as India’s ninth most frequent cause of mortality.
Liver cirrhosis causes
Alcohol misuse, persistent liver virus infections (hepatitis B and hepatitis C), fatty liver linked to obesity, and diabetes can all aggravate liver cirrhosis. Cirrhosis can be brought on by anything that harms the liver. Alagille syndrome (born with fewer bile ducts than normal), jaundice, auto-immune disorders, hemochromatosis (excess iron found in the liver), Wilson disease (excess copper found in your liver), cystic fibrosis, glycogen storage diseases (liver can’t store or break down glycogen), etc.
Additionally, primary biliary cholangitis (permanent bile ducts damage), primary sclerosing cholangitis (bile duct inflammation & scarring, narrowing the ducts), blocked bile duct, biliary atresia (infants with blocked bile ducts, causing damage, scarring), chronic heart failure (causes fluid to back up in your liver, swelling in other areas of your body and other symptoms), rare diseases, such as amyloidosis, etc. also can disrupt normal liver function leading to complications in future.
Cirrhosis develops throughout time as a result of progressive liver disorders. Liver cells begin to die when they are harmed and if the injury persists. Over time, the liver’s injured cells are replaced by scar tissue, impairing its ability to operate. Additionally, liver damage may be caused by viral hepatitis, long-term diabetes, obesity, unprotected sex, and other factors.
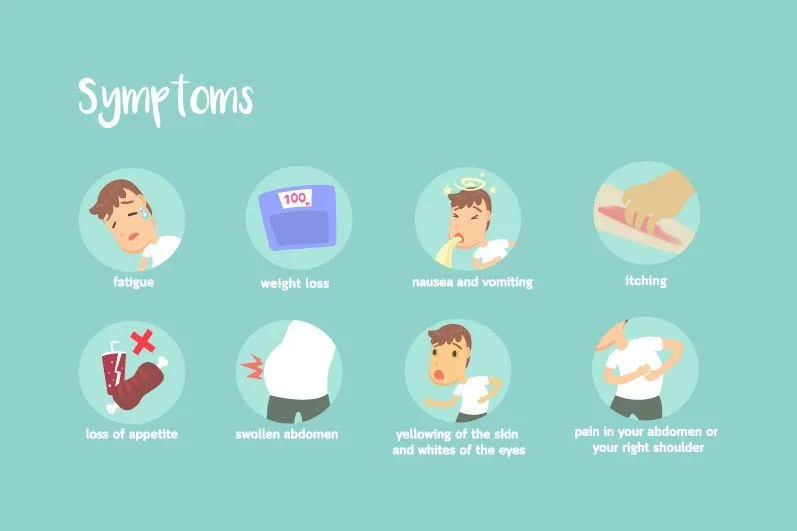
Liver cirrhosis symptoms
The stage of your liver condition will decide your cirrhosis symptoms. You might not exhibit any signs in the early stages. If you experience symptoms, some may be generic and readily confused with those of a wide range of other conditions. Loss of appetite, weakness, fatigue, nausea, fever, sudden weight loss, easy bleeding and bruising, jaundice, itchy skin, edema in the legs, feet, and ankles, fluid build-up in the abdomen (ascites), brownish or orange urine, light-colored stools, confusion, difficulty thinking, memory loss, personality changes, blood in the stool, redness in the palms of the hands, and spider-like blood vessels that surround tiny, are just a few of the (telangiectasias). For men, we observe the loss of sex drive, enlarged breasts (gynecomastia), shrunken testicles, etc. In women, premature menopause.
Types of cirrhosis
There are three macroscopic kinds of liver disease, including micronodular, macronodular, and mixed cirrhosis, depending on the size of the nodules. Regenerating nodules will be less than 3 mm in the Laennec’s cirrhosis or portal cirrhosis micronodular type. The nodules in macronodular cirrhosis (post-necrotic cirrhosis) are greater than 3 millimeters.
There are two different types of cirrhosis: alcoholic and non-alcoholic. Hepatitis B and C are the viruses that most frequently lead to cirrhosis in the non-alcoholic variety around the world. Still, hepatitis A and D are also known to cause severe liver scarring, albeit rarely.
Hepatitis A, B, and C are viral infections. Primary biliary cholangitis and auto-immune hepatitis are auto-immune liver cirrhosis variants. Hemochromatosis and Wilson disease are two examples of inherited liver conditions. Liver carcinoma also can lead to cirrhosis. Further, alcohol abuse leads to alcoholic fatty liver disease. Overeating fat causes non-alcoholic fatty liver disease (NAFLD). As the prevalence of obesity and diabetes rises, NAFLD is becoming more widespread.

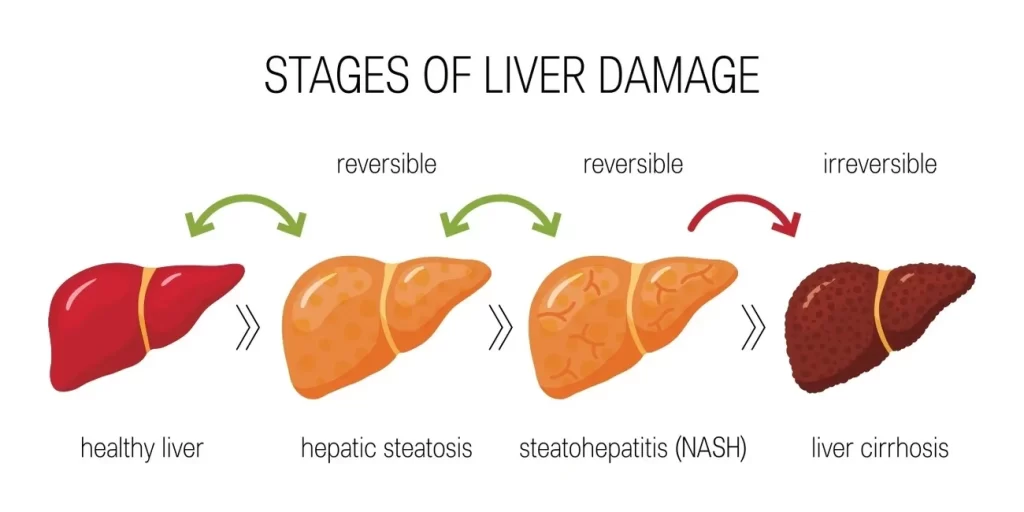
Liver cirrhosis stages
Compensated cirrhosis and decompensated cirrhosis are the two stages of the disease (clinical stages). Although the stages are dynamic and progressive, it is possible to reverse the process from the stage of decompensation to the stage of compensation. Asymptomatic compensated cirrhosis is the condition. Patients who have received compensation don’t have jaundice, hepatic encephalopathy, ascites, or variceal bleeding. Patients with compensated cirrhosis have a median survival span of more than 12 years.
Cirrhosis has four phases, including
Stage I, which is steatosis or inflammation of the bile duct or liver, which characterizes the initial stage of liver disease.
Stage II: Liver fibrosis (scarring) brought on by inflammation. As good tissue is replaced by scarred tissue, your liver’s ability to operate properly is reduced.
Stage lll – The liver is severely scarred. At the cirrhosis stage, further liver damage symptoms, such as jaundice, weakness, fatigue, loss of appetite and weight, abdominal bloating, and edema in your extremities may be present.
Stage IV: Advanced liver disease, hepatic failure, or liver failure.
Alcoholic cirrhosis
Acute liver inflammation is caused by alcoholic hepatitis. When normal liver tissues are destroyed, liver cells die, frequently followed by persistent scarring. The functioning liver tissue is replaced by scar tissue. There might not even be any noticeable symptoms at this point. Although it’s usually irreversible, quitting consuming alcohol right now can avert future harm and greatly lengthen your life.
15% of patients with alcoholic cirrhosis will develop hepatocellular carcinoma, and two-thirds of these patients had decompensated disease at presentation. At five years, survival rates range from 0% to 80%, and 60–90% of people die of liver disease. Some alcoholics may have severe physical and psychological symptoms of alcoholism without experiencing significant liver damage. Alcoholic cirrhosis is found among alcoholics about 10 to 25 percent of the time.
Non-alcoholic cirrhosis of the liver
The phrase “non-alcoholic fatty liver disease” (NAFLD) refers to a number of ailments brought on by an accumulation of fat in the liver. Obese or overweight people frequently exhibit it. The majority of the time, early-stage NAFLD is harmless, but if it worsens, it can result in severe liver damage, including cirrhosis. Additionally linked to an increased risk of significant health issues like diabetes, high blood pressure, and renal disease are high levels of fat in the liver.
NAFLD raises your risk of getting cardiac problems if you already have diabetes. If NAFLD is detected and treated early, you can stop it from getting worse by reducing the amount of fat in your liver. Typically, without being aware of it, the majority of people will only ever reach the first stage. If it’s not identified and treated, it can occasionally worsen and result in liver damage.
Simple fatty liver (steatosis), a relatively harmless accumulation of fat in the liver cells that can only be detected during tests conducted for another cause, is one of the main stages of NAFLD.
Non-alcoholic steatohepatitis (NASH) is a severe variant of NAFLD in which the liver has inflammatory changes. If you have type 2 diabetes, insulin resistance, polycystic ovary syndrome, underactive thyroid, high blood pressure, high cholesterol, metabolic syndrome, are above the age of 40 years, are obese or overweight, or have any of these conditions, you are at an increased risk of developing NAFLD. However, NAFLD has been identified in patients, including young children, who do not have any of these risk factors. NAFLD is not brought on by excessive alcohol consumption, even though it closely resembles alcohol-related liver disease (ARLD).
I. Primary biliary cirrhosis
The bile ducts in your liver are gradually destroyed by primary biliary cholangitis, formerly known as primary biliary cirrhosis. What causes bile duct inflammation is not known clearly. Primary biliary cirrhosis, however, is an auto-immune disease. Cholestasis is typically one of the symptoms (accumulation of bile in the liver).
In this situation, you should refrain from consuming raw or undercooked shellfish, fish, meat, and unpasteurized milk. In persons with liver illness, bacteria or viruses from these foods can lead to serious infections. Bile can be restored in the liver and harm liver cells when bile ducts become compromised. Failure of the liver may be the result.
II. Nash cirrhosis
In addition to liver fat, NASH (Non-Alcoholic Steato Hepatitis) is a variant of NAFLD in which the liver is also inflamed and damaged. NASH can result in liver fibrosis or scarring due to the inflammation and liver damage it causes. NASH may result in cirrhosis, a condition in which the liver is permanently scarred. For people with decompensated liver failure, the typical survival time is two years. The most severe type of non-alcoholic fatty liver disease, NASH, can also result from metabolic disease.
NASH alone may not be fatal, but its coexistence with other risk factors, such as advanced age and diabetes, may raise the possibility of end-stage liver disease, a fatal illness. Occasionally, persons with liver fat develop NASH. NASH patients may experience symptoms that take months or even years to manifest. Diabetes, high cholesterol, high triglycerides, poor nutrition, metabolic syndrome, polycystic ovarian syndrome, sleep apnoea, hypothyroidism, and other conditions are also causes and risk factors for NASH.
III. Cryptogenic cirrhosis
Patients with cryptogenic cirrhosis, a disorder that inhibits liver function and is often diagnosed in mid-to-late adulthood, acquire permanent liver disease brought on by liver scarring. Non-alcoholic steatohepatitis is expected to have a significant role in cryptogenic cirrhosis, despite the fact that the actual origin is unknown. Obesity, hyperlipidemia, and metabolic issues like diabetes have all been linked to the emergence of this illness.
Clear clinical distinctions between cryptogenic cirrhosis and cirrhosis from other sources were discovered. As a result, NASH cirrhosis and cryptogenic cirrhosis should not be confused. In order to determine cirrhosis’s unidentified causes, more research is necessary. Liver function is compromised by a disorder called cryptogenic cirrhosis. People with this stage develop the irreversible liver disease by scarring of the liver, typically in mid-to-late adulthood.
IV. Compensated cirrhosis
Compensated cirrhosis is typically asymptomatic in nature. Patients who have compensated stage don’t have jaundice, hepatic encephalopathy, ascites, or variceal hemorrhage. Life expectancy for those with compensated cirrhosis is between 9 and 12 years, however, they do not experience symptoms. Although 5-7% of persons with the illness will experience symptomatic onset each year, a person can stay asymptomatic for years.
Patients who have cirrhosis in its early stages are more likely to have it reverse. Although the exact point at which cirrhosis becomes irreversible is unknown, it appears that it does so once septal neovascularization has place and portal pressure dramatically rises. Any form of liver injury can cause scarring, which could eventually develop into decompensated cirrhosis. Sometimes, anti-viral medicines which is used to treat hepatitis C can aggravate hepatitis and the only way is to stop this medication, so as to reduce further damage.
V.Decompensated cirrhosis
Decompensated cirrhosis is characterized by jaundice, ascites, hepatic encephalopathy, hepatorenal syndrome, or variceal hemorrhage and is defined as an acute decline in liver function in a patient with cirrhosis. The typical life expectancy for those with decompensated cirrhosis is between 1 and 3 years. Age, general health, and potential issues including the intensity of symptoms and other disorders all play a role in this.
The stage that follows compensated cirrhosis is known as decompensated cirrhosis. As a result of excessive scarring of liver, problems arise. Hepatorenal syndrome, or kidney failure in liver disease, is a dangerous consequence that can affect people with decompensated cirrhosis who are already seriously ill with issues like encephalopathy, jaundice, and bleeding problems. Most patients require a liver transplant, and some people require one right away. Decompensated cirrhosis has few therapeutic alternatives. Most of the time, liver disease cannot be reversed at this advanced stage. However, it also means that those who have decompensated cirrhosis are frequently excellent candidates for liver transplants.
VI. Cardiac cirrhosis
The phrase “cardiac cirrhosis” is used to describe a range of hepatic illnesses that develop as a result of hepatic congestion brought on by cardiac malfunction, particularly in the right heart chambers. Symptoms of this illness include leg oedema, orthopnoea, paroxysmal nocturnal dyspnoea, and shortness of breath.
Valvular disease, severe pulmonary hypertension, cor pulmonale, biventricular heart failure, pericardial disorders, cardiac tamponade, constrictive pericarditis, and other cardiac abnormalities are common causes of cardiac cirrhosis. Additionally, liver function with regard to synthesis may be compromised, which could result in transplant-related bleeding issues. The synthetic function, however, considerably improve within 3 months of the transplant, according to a study looking at the reversibility of cardiac cirrhosis in patients receiving heart transplants. Most patients with cardiac cirrhosis don’t exhibit any symptoms. Usually, abnormal liver function tests will indicate this problem. Breathlessness, limb oedema, paroxysmal nocturnal dyspnoea, and orthopnoea are common signs of heart failure.
Liver cirrhosis treatment
The major therapies for cirrhosis involve reducing your salt intake and using a kind of medication known as a diuretic, like spironolactone or furosemide. You could require antibiotics if the fluid in your stomach develops an infection. In extreme circumstances, you might need to have a tube inserted to drain the fluid from your stomach region.There are numerous lifestyle adjustments you can do if you have cirrhosis to lower your risk of developing new issues and complications. These include abstaining from alcohol, giving up smoking, losing weight if you’re overweight or obese, exercising regularly to prevent muscle loss, maintaining good hygiene to lower your risk of infection, etc.
A doctor may request blood tests to look for any enzymes that might point to liver damage as well as for indicators of liver dysfunction, such as excess bilirubin. Your blood is examined for creatinine levels to determine renal function. You’ll undergo testing for hepatitis viruses. Your blood’s capacity to clot is also assessed using your international normalised ratio (INR). Doctors may be able to identify the underlying cause of cirrhosis based on the findings of a blood test. In order to determine the severity of your cirrhosis, we need to have proper blood tests.
It could be advised to undergo imaging tests like magnetic resonance elastography (MRE). This non-invasive, sophisticated imaging examination finds liver stiffening or hardening. The use of other imaging tests including MRI, CT, and ultrasound is also possible.
Biopsy : A tissue sample is not always required to make a diagnosis (biopsy). However, it might be used by your doctor to determine the degree, scope, and origin of liver damage.By treating the underlying cause in early cirrhosis, the liver’s damage may be reduced. There are options for alcohol dependency therapy. People who have cirrhosis brought on by binge drinking should make an effort to cut back. A medical professional may suggest an alcohol addiction treatment programme if quitting drinking is challenging. It is imperative to avoid drinking if you have cirrhosis since alcohol is poisonous to the liver in any proportion.
Weight loss. Losing your body weight and managing your blood glucose levels may improve the health of those with cirrhosis brought on by non-alcoholic fatty liver disease.

Through targeted therapy of the hepatitis B or C viruses, medications may prevent further harm to liver cells caused by these viruses. Sometimes, the very medications used to treat further cirrhosis aggravate cirrhosis. The progression of some kinds of liver cirrhosis may be slowed by medication. For those with primary biliary cirrhosis who receive an early diagnosis, treatment may greatly slow the development of cirrhosis. Certain symptoms, such as itching, exhaustion, and discomfort, can be treated with other drugs. Nutritional supplements may be administered to avoid weak bones and to combat the starvation brought on by cirrhosis (osteoporosis).
Certain antihypertensive drugs can manage elevated pressure in the veins that supply the liver (portal hypertension) and stop life-threatening haemorrhage. A regular upper endoscopy will be done by the doctor to check for varices (swollen veins in the oesophagus or stomach that could bleed).
To lessen the danger of bleeding, you probably require medicine if you develop varices (enlarged or swollen veins). You might require a procedure (band ligation) to stop the bleeding or lower the risk of further bleeding if you have symptoms indicating that the varices are bleeding or are likely to haemorrhage. In extreme circumstances, a tiny tube called a trans jugular intrahepatic portosystemic shunt may need to be implanted in your vein to lower liver blood pressure.
Infections: Antibiotics or other therapies may be used to treat infections. Additionally, your doctor may advise immunizations against hepatitis, pneumonia, and influenza. increased risk of liver cancer. The doctor would probably advise routine blood tests and ultrasounds to check for liver cancer symptoms.
Hepatic encephalopathy – Doctor might recommend drugs to assist lower the accumulation of toxins in your blood brought on by poor liver function.
Surgery for a liver transplant may be the sole option for treating severe cirrhosis when the liver no longer functions. With a liver transplant, your damaged liver is replaced with a healthy liver from a deceased donor or with a portion of a living donor’s liver. One of the most frequent indications for a liver transplant is cirrhosis. In order to evaluate whether liver transplant candidates are healthy enough to recover well from surgery, they must undergo a battery of tests.
Ursodeoxycholic acid 300 mg
Indications of Ursodeoxycholic acid 300 mg is prescribed for primary biliary cirrhosis and to dissolve small to medium-sized radiolucent, cholesterol-rich gallstones in people with a functional gall bladder. UCDA does not dissolve calcium-coated cholesterol stones or stones made of bile pigments. In the treatment of individuals for whom surgery is either contraindicated or who are anxious to avoid surgery, UDCA is the right choice. Although the effects of this medication on the liver have not yet been proven clearly, it has anti-apoptotic, cytoprotective, anti-oxidative, immunomodulatory, and membrane-stabilizing properties.
Hepatobiliary disorders in children aged 6 to under 18 years are linked to cystic fibrosis in the paediatric population. The recommended dose for adults and the elderly is 10–15mg of UDCA per kg per day, divided into two–four doses. Children: The dosage ought to be based on body weight.
Adults and the elderly should typically take 6 to 12 mg/kg/day, either all at once at night or in divided doses, to dissolve gallstones. If necessary, this might be raised to 15 mg/kg/day for people who are obese. Depending on the size of the stones, the course of therapy could last up to two years. It should also be continued for a further three months after the stones appear to have disappeared.
Children: Dosage should be related to bodyweight. Children with cystic fibrosis who are 6 years old to under 18 years old should receive 20 mg/kg/day in 2-3 divided doses, with an additional increase to 30 mg/kg/day if necessary.
Possible side effects of ursodeoxycholic acid
The majority of people taking this medicine may not have any negative side effects. They are mild to moderate adverse effects that progressively fade away. You might need to see a doctor if they last longer than expected or start to get worse. Ursodeoxycholic Acid Tablets 300 Mg’s most frequent side effects include stomach pain, nausea, rashes, hair loss, itching abdominal pain, and bladder pain. Other side effects include bloody or cloudy urine, difficult, burning, or painful urination, fast heartbeat, frequent urges to urinate, severe nausea, skin rash or itching over the entire body.